How are my brain and syrinx looking 3 months post-op?
Hey y'all, it's been a while since I made an official post! I wanted to update you on how my three-month check-in went and what this means for the future! So here it is:
My MRI took place at the outpatient facility of my hospital at 10 AM on February 18, 2025. I told my doctor beforehand that I have claustrophobia since I have a lot of trouble staying still during my scans, so they gave me 5 mg of diazepam to take 30-60 minutes before the MRI, which was a HUGE help. I usually get really squirmy in the machine, but I was asleep on and off through my entire scan this time. So if you have had a similar experience, I highly recommend informing your doctor to see what they can do to help.
My scan took about an hour and a half, and my 3-month follow-up with my neurosurgeon was at 1 PM, so my dad and I went to grab a quick lunch at the hospital cafeteria. While walking to the outpatient center after eating, I saw my results were uploaded to my patient portal, so I peeked before my appointment (even though I knew I should have waited).
The amazing news: My cerebellum looks phenomenal.
I am so glad we did each surgical intervention because it seems like each element contributed to me having such a great outcome. By removing the suboccipital skull and C1 lamina, there is now less external compression from the bone, which stops the tonsils from being pushed so hard. By placing a dural graft over my spinal cord, the space for CSF to flow around my tonsils is greater. By having my cerebellar tonsils cauterized, there is less tonsil to create the peg-like obstruction out of my foramen magnum. Reading the words "resolution of previously seen peglike appearance of the cerebellar tonsils and crowding at the foramen magnum" on my report was absolutely surreal. I want to make that into a neon sign or a throw pillow and put it in my apartment so I can see it every day.
I did not expect there to be this much of a gross difference in the appearance of my cerebellum and CSF flow because my incision site and the scale of the surgery were so small. I even thought with how unpredictable scarring can be that my tonsils might end up more herniated. But check it out for yourself! My favorite image is Figure 4.
Figure 2. Notable changes on my 3-month T1 MRI from Figure 1 indicated with color. The areas of suboccipital craniectomy and C1 laminectomy can be seen with the purple overlay in the dark area beside my skull and the absence of the triangle-shaped bone (C1 lamina) to the right of my spinal cord in the pre-surgery image. My remaining cerebellar tonsil is emphasized with the teal overlay.
Figure 3. T2 MRI of my brain 3 months post-op. The new region of CSF flow can be seen with the yellow overlay. The remaining cerebellar tonsil is emphasized with the teal overlay.
More amazing news: Absolutely NO restrictions!!
Dad even asked if I could become a powerlifter now (he was joking, y’all have seen my arms), and my neurosurgeon said I could if I felt so inclined. So bring on the Valsalva maneuvers! His guidelines are to increase activity slowly as tolerated, and if it hurts, slow down a little. Another thing for me to keep in mind is that I *did* have the muscles attaching to the back of my skull cut for the procedure. Because of this, these muscles will always be more sensitive to injury. So if I do something a little hardcore and feel a tweak, I probably didn’t do something awful, just strained my neck.
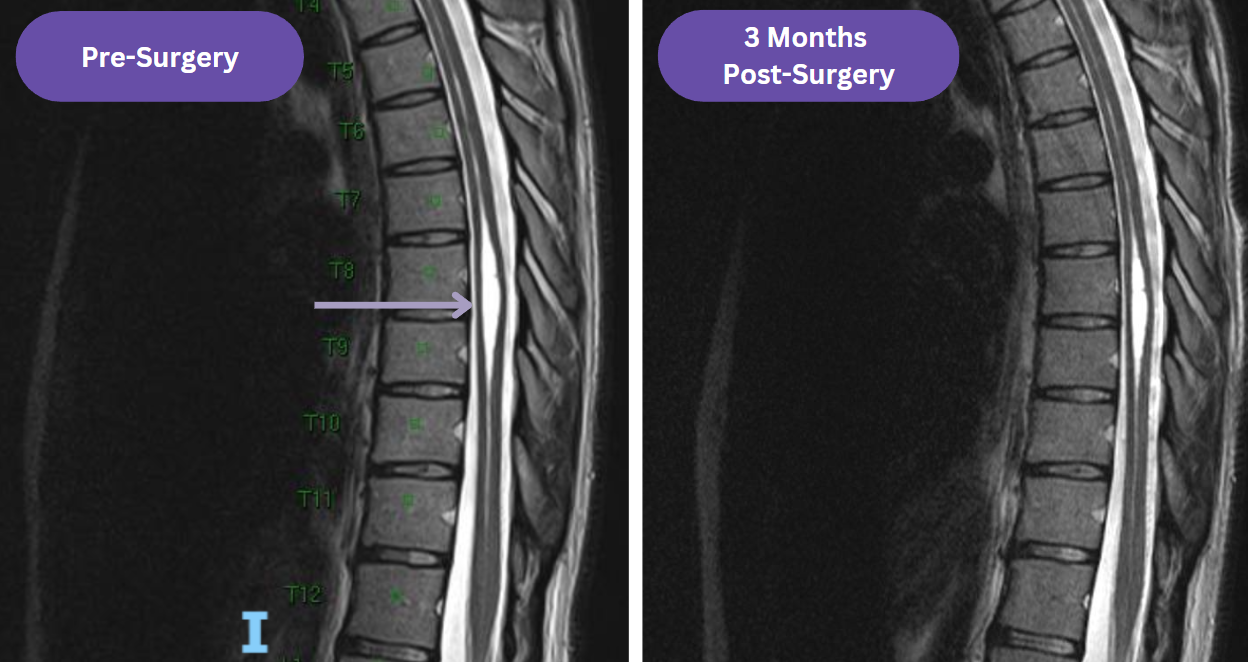
The not-horrible-but-not-amazing news: My syrinx does not look much better.
The MRI report noted there was a decrease in the width of my syrinx from 7 mm to 6 mm. But since the improvement was hard to see at first glance, I was pretty bummed. The length of my syrinx is the same as pre-surgery, extending from my cervical to my lumbar region. However, when reviewing my MRI, my doctor said that even though he wished my syrinx was smaller too, he “wouldn’t lose sleep over it,” which was very encouraging. He let me know we could still see some improvement over the next year. Since the widest part of my syrinx is so low in my thoracic spine, it could take longer to see changes. Furthermore, since I am not experiencing sensation or temperature loss in the T7 region or below, he is confident that my symptoms are not related to my syrinx, which is fantastic. So we are planning to keep monitoring if the syrinx progresses with annual physical exam and MRI.
Figure 5. Comparison of my syrinx in November 2024 versus February 2025 up close around T7-T9.
Figure 6. Me before my MRI with only a little less hair and A LOT less cerebellar tonsil than my last hospital gown pic!
The current plan is that I will be having an in-person visit with my neurosurgeon again in November 2025 for a one year check-in. I’ll also be getting a brain and cervical, thoracic, and lumbar spine MRI.
Afterthoughts
Now that I’ve had some time for the initial emotions to settle, I feel very optimistic and excited to start seeing what my body can do again. Even though my syrinx did not improve much, I am hopeful that the cause of my symptoms is resolved since I am feeling so much better and my cerebellum and the surrounding area look so different. Leaning on the scientific method and the words of my amazing neurosurgeon, I am hopeful that this is the beginning of a new era of my life.
Since surgery, I have kind of felt like I’m in a dream sequence because I have felt so much better than I have in years, so I don’t fully trust it yet. I’ve been waiting to wake up in that same level of pre-surgery pain again and be back to square one because of so many attempted and failed treatment plans before getting to my diagnosis. So I’m going to work toward trusting my body again and use my time off to set some goals and get excited about both the present and the future.
Goals
Now that I’m officially off restrictions, I want to make the most of this time leading to rotations in May. So here are some things I want to do with this unique runway of time before getting back into the grind:
- Get back to the gym again (once a week to start).
- Really enjoy this time off with my loved ones.
- Continue my physical therapy maneuvers since they’ve been so great for me, especially for my neck.
- Continue completing all my appointments so I can go back to school as healthy as possible.
- Keep that same “you never know when you could start feeling like garbage again, so enjoy today as much as possible” energy, but also let myself celebrate the idea that this healthy, able-bodied state I’m in may get to be my new normal.
- Keep it up with my Chiari research projects.
- This research and working with patients with underrepresented conditions makes me feel such a strong sense of purpose. I’m planning on keeping it up while I’m in med school as well!
- Start inching my way back into relearning medicine- nothing crazy, but a little review and some practice questions here and there to gear up for returning to school in May.
I’ll keep you all updated with my pain levels, wins, goal adherence, and everything I’m up to HERE. Feel free to reach out with any questions or thoughts :) As always, I absolutely LOVE hearing from you all!
Glossary
T1 MRI: an MRI viewing technique that makes fat appear bright white and fluid, air, and bone appear dark
T2 MRI: an MRI viewing technique that makes fat appear dark and fluid, air, and bone appear bright white
Valsalva maneuver: a breathing technique where an individual forcefully exhales while their airway is closed to increase chest pressure, which often causes a worsening of symptoms in Chiari patients








Comments
Post a Comment